
Written by Dr Ryan Lee, Consultant obstetrician and Gynaecologist Specialist
Antenatal screening tests for fetal abnormalities help detect complications during pregnancy and consequently allow pregnant women to receive appropriate care and follow-up for their pregnancies. Prior knowledge about antenatal screening allows parents to prepare them physically and emotionally better to make decisions about the pregnancy.
Antenatal tests can broadly be categorised as non-invasive or invasive. The non-invasive test includes the OSCAR One-Stop Clinic for Assessment of Risk test) and NIPT (Non-Invasive Prenatal Test). Invasive tests include amniocentesis and chorionic villus sampling.
OSCAR Test
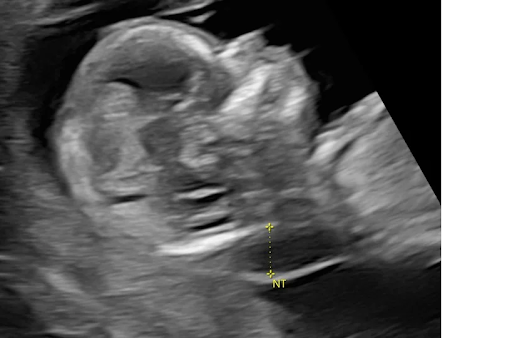
The OSCAR (One-Stop Clinic for Assessment of Risk test) involves a nuchal translucency (NT) ultrasound scan assessing the thickness of skin in the neck of the fetus between 11 – 13 weeks of gestation and a blood test.
The majority of fetuses with Increased nuchal translucency (NT) detected are normal. However, they may also be associated with chromosomal abnormalities such as Down Syndrome, genetic syndromes, and structural abnormalities such as heart problems.
The combined results are analysed with a computer algorithm software and a ‘risk score’ is calculated. Its accuracy is around 85-90% and it also has a zero risk of harm to the fetus.
If a fetus is screened for high risk during the OSCAR test, pregnant mothers will be referred for further tests such as the Non-Invasive Prenatal Test (NIPT), a screening test with 99% detection for Down syndrome and/or invasive test with chorionic villus sampling around 11-14 weeks gestation or amniocentesis from 15 weeks gestation for diagnosis.
The combined results are analysed with a computer algorithm software and a ‘risk score’ is calculated. Its accuracy is around 85-90% and it also has a zero risk of harm to the fetus.
If a fetus is screened high risk during the OSCAR test, pregnant mothers will be referred for further tests such as the Non-Invasive Prenatal Test (NIPT), a screening test with 99% detection for Down Syndrome and/or invasive test with chorionic villus sampling around 11-14 weeks gestation or amniocentesis from 15 weeks gestation for diagnosis.
Non-Invasive Prenatal Test (NIPT)
- NIPT is a blood test is used to detect fetal cell free DNA within the mother’s blood from 10 weeks of pregnancy onwards.
- Most results will be returned within 5-7 days.
- NIPT can also reveal the gender of the baby.
- NIPT has zero risk of harm to the fetus.
- NIPT is the most sensitive screening test for the common chromosomal abnormalities like Down syndrome (Trisomy 21), Edward syndrome (Trisomy 18) and Patau Syndrome (Trisomy 13).
- NIPT can also detect several rare microdeletion genetic syndromes.
- Although NIPT is highly accurate (up to 99% for Down syndrome), it is still a screening test and not a diagnostic test. A high risk result means that your pregnancy has a higher chance of having a specific genetic condition. However, you cannot know for sure if your baby has that condition based on screening results alone.
- If the results of NIPT suggest the fetus has a suspected chromosomal or genetic disorder, a diagnostic test like chorionic villus sampling (CVS) or amniocentesis is required to confirm the diagnosis.
- About 1 in 65 women could receive a no result or other type of result such as inconclusive results. Your doctor will discuss with you about having a second blood redrawn to do the test again. There is still a 20% chance of further no result or a small chance that NIPT will have a result relating to your genetics or your physical health.
Pre-eclampsia screening
Pre-eclampsia is a pregnancy complication with high blood pressure that occurs after 20 weeks of pregnancy; often associated with proteins in the urine, biochemical abnormalities, organ damage and/or fetal growth restriction.
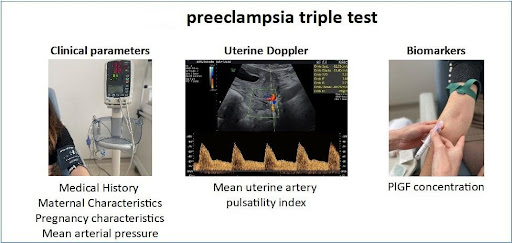
First trimester screening for pre-eclampsia at 11-13 weeks gestation identifies women with an increased risk of developing pre-eclampsia. Pre-eclampsia screening can be performed together with OSCAR (One-Stop Clinic for Assessment of Risk test).
These various tests include
- Maternal risk factors such as age, history of hypertension, pre-eclampsia, diabetes, lupus, or chronic kidney disease and measurement of mean arterial pressure.
- Ultrasound measurements using uterine artery doppler studies to assess blood flow in the uterine arteries
- Biomarkers such as PAPP-A (Pregnancy-associated Plasma Protein-A) and PLGF ( placenta growth factor) are taken during 11-13 weeks gestation in combination with the OSCAR test.
First trimester screening for pre-eclampsia is not a definitive diagnosis but a useful screening test to identify women at high risk of developing pre-eclampsia before 37 weeks.
Further diagnostic tests or close antenatal monitoring may be recommended based on results to early detect and manage pre-eclampsia. Currently, the only known treatment of pre-eclampsia is delivery and this may warrant earlier delivery in pre-eclampsia.
If the risk of pre-eclampsia is high < 1:100, calcium supplementation of at least 1 g / day and low dose aspirin of 150 mg taken at night from 12 weeks gestation reduces the risk of this complication by about 60% before 37 weeks gestation.
A comparison of Antenatal Tests
| Test | Type | Timing | Detection rate | Costs | Remarks |
| Nuchal translucency alone ( NT) | Ultrasound | 11-13 weeks | 50-60% | Screening tests for both structural and chromosomal problems with lower accuracy | |
| OSCAR | Ultrasound + Blood | 11-13 weeks | 80-85% | Screening tests for both structural and chromosomal problems with higher accuracy than NT alone | |
| NIPT | Blood | 10 weeks onwards | 93-99% | More accurate for screening chromosomal problems and microdeletion genetic syndromes.
Able to reveal gender Does not detect structural problems Possibility of no result |
|
| Pre-eclampsia screening | Ultrasound + Blood | 11-13 weeks | 75% | Screens for Pre-eclampsia <37 weeks,
cut off positive risk 1:100 recommend aspirin 150 mg once a night till 36 weeks |
|
| Amniocentesis/chorionic villus sampling | Invasive | 11-15 Weeks onwards | 100 % | Invasive diagnostic test
1/300 risk of miscarriage Result up to 2 weeks |






